Mortality according to the cumulative time at different systolic blood pressure levels in critically ill patients: a retrospective cohort study.
Jian-Bin He, MD1, 2, 3, Yue Shang, RN1, 2, 3 ,Ming-Yu Xu, MD1, 2, 3 ,Lin Yuan, MD1, 2, 3 ,Dai-Qiang Huang, MD1, 2, 3 ,An-Min Hu, MD1, 2, 3*, Jian Huo, MSc4
1 Department of Anesthesiology, Shenzhen People's Hospital, Shenzhen, China. 2 The Second Clinical Medical College, Jinan University; Shenzhen, China. 3 First Affiliated Hospital, Southern University of Science and Technology, Shenzhen, China. 4 Boston Intelligent Medical Research Center, Shenzhen United Scheme Technology Co., Ltd. Corresponding authors at: Boston Intelligent Medical Research Center, Shenzhen United Scheme Technology Co., Ltd. 101 Federal Street, Suite 1900, Boston, Massachusetts, 02110. Tel: 1-972-299-8414; E-mail addresses: huojian@szus.org (J. Huo)
Abstract
Background: Previous research has shown a non-linear relationship between systolic blood pressure (SBP) and patient outcomes, with increased risks at both low and high SBP levels. However, the specific association between different SBP levels and outcomes in critically ill patients remains unclear. This study aimed to investigate the relationship between the cumulative time spent at various SBP levels and mortality in this patient population.
Methods: A retrospective analysis was conducted using data from the MIMIC-III database, encompassing over 3 million SBP records from 30,833 patients. The associations between cumulative time spent within four SBP ranges (<100, 100-120, 120-140, and ≥140 mmHg) and 12-month mortality were evaluated. Restricted cubic splines and multivariable Cox regression models were employed to assess the relationships between the percentage of cumulative time at different SBP levels (categorized into four levels: <25%, 25-50%, 50-75%, and ≥75%) and mortality after intensive care unit (ICU) admission.
Results: The study found that prolonged periods with SBP <100 mmHg were associated with a higher risk of mortality, while time spent with SBP within the 120-140 mmHg range was associated with reduced mortality risk. Patients spending the highest percentage of cumulative time at SBP <100 mmHg exhibited an approximately 4.24-fold increased risk of 12-month mortality compared to those in the lowest percentage category. Conversely, patients with the highest percentage of cumulative time at SBP 120-140 mmHg demonstrated a lower adjusted risk of mortality at 12 months (OR, 0.49; CI, 0.42-0.56) compared to those in the lowest percentage category.
Conclusion: The results of this study suggest that for critically ill patients, SBP <100 mmHg is associated with increased mortality following ICU admission, whereas maintaining SBP within the 120-140 mmHg range may lead to improved outcomes. Further research, specifically randomized trials, is necessary to establish whether interventions targeting this optimal SBP range after ICU admission can effectively enhance patient outcomes.
Key words: Systolic Blood Pressure, Mortality Benefit, Risk Exposure, Critically Ill Patients.
Introduction
Systolic blood pressure (SBP) is a pivotal factor in patient outcomes, with appropriate management crucial for improving patient well-being (1–5). A J-shaped relationship has been established between SBP levels and the occurrence of cardiovascular events and overall mortality (6–8). Notably, the total duration of hypotension has been linked to an elevated risk of death (2,9,10).
Prior studies have shown that a rapid drop in systolic blood pressure (SBP) within the first 24 hours after admission for acute heart failure is linked to worsened outcomes within the first 6 months, including kidney problems (11). Similarly, in patients with stable heart disease or elevated cardiovascular risk, lowering SBP below 120 mmHg during treatment has been associated with an increased risk of death (6,12). Notably, the optimal baseline SBP for minimizing risk in high-risk patients appears to be within the range of 120 to 140 mmHg (7,13).
While maintaining appropriate arterial pressure may potentially enhance the prognosis of critically ill patients, research investigating this association remains limited. This study aims to address this knowledge gap by examining the relationship between the duration of various SBP levels and mortality rates in critically ill patients. The findings of this study will inform the development of evidence based SBP management strategies following admission to the intensive care unit (ICU).
Methods
This study utilized data from the Multiparameter Intelligent Monitoring in Intensive Care III (MIMIC-III) database (version 1.4), curated by the Laboratory for Computational Physiology at the Massachusetts Institute of Technology (14). This database comprises de-identified electronic health records of over 46,500 critically ill patients admitted to intensive care units (ICUs) at Beth Israel Deaconess Medical Center between 2001 and 2012. Due to the de-identified nature of the data and researcher completion of human subjects training, ethical approval and informed consent were waived for this study.
Study population and stratification.
Inclusion criteria were: (1) only the first ICU stay for patients with multiple admissions, (2) age 18-89 at ICU admission, (3) ICU stay ≥24 hours, and (4) inclusion of all recorded SBP measurements (both noninvasive and invasive) during the ICU stay. Noninvasive blood pressure (NIBP) values outside the physiological range (<20 mmHg or >300 mmHg) were excluded. If NIBP and invasive blood pressure (IBP) measurements were available at the same time point, the higher value was selected.
Total SBP measurement hours were calculated and categorized into four ranges: <100-120, 120-140, and ≥140 mmHg. Additional variables extracted from the database included demographics, fluid balance parameters, laboratory test results, mechanical ventilation duration, and vasoactive drug use.
Outcomes
The endpoint was the 12-month mortality after ICU admission.
Data analysis
Continuous variables were summarized using medians and interquartile ranges (IQRs). Categorical variables were presented as frequencies and percentages. Comparisons of patient characteristics between groups were performed using chi-square tests for categorical variables and either unpaired t-tests or Kruskal-Wallis tests for continuous variables, depending on the normality of the data distribution. Missing data for patient characteristics were imputed using random forest algorithms (15).
Cumulative time spent within each SBP range was measured in hours. The percentage of cumulative time in each range was categorized into four levels: <25% (level I), 25-50% (level II), 50-75% (level III), and 75-100% (level IV).
Overall survival, defined as the time from admission to the ICU until death from any cause, was estimated using the Kaplan-Meier method. Statistical differences in survival between groups were assessed using a stratified log-rank test. Restricted cubic splines were employed to model the relationship between the percentage of cumulative time at different SBP ranges and mortality risk.
Multivariable Cox proportional hazards regression models were used to examine the associations between cumulative time at different SBP ranges and mortality. Covariates included patient characteristics, fluid balance parameters, laboratory values, mechanical ventilation duration, and vasopressor use. All results presented are from the fully adjusted model. All analyses were performed using R version 3.61.
Results
Among the 46,428 ICU patients and 61,051 ICU admissions in the MIMIC-III v1.4 database, 6,736,615 SBP records were available. Sequentially, we excluded 9,948 patients whose age at admission was above 89 years or below 18 years and 5,647 patients who stayed in the ICU less than 24 hours, as illustrated in (figure 1). The final cohort comprised 30,833 patients with their first ICU admission and the corresponding 3,711,495 records of SBP measurement.

Figure 1. The flow of participants through the study. ICU, intensive care unit; SBP, systolic blood pressure
The 12-month mortality rate of patients after admission to the ICU was 21.5% (n=7,866). Overall, fatal patients were older, had a higher SAPS-II score during first day of admission, and have longer ICU stay and hospital stay than survival patients (Table 1)
Kaplan-Meier curves showed the association of the percentage of cumulative time at SBP levels with all-cause death (Figure 2). The difference in overall survival at the four levels was statistically significant (P <0.001 by the log-rank test).
Table 1. Data Set Population Characteristics and Characteristics of Patients who survived and died 12-month after admitting to ICU.

Analysis taking the percentage of cumulative time at different SBP levels as a continuous variable and using cubic spline regression revealed that the relationship between the percentage of cumulative time and mortality was nonlinear. (Figure 3) shows the HRs for 12-month mortality and the percentage of cumulative time at different SBP levels after adjusting for all variables in the table. Twenty-five percent of the cumulative time was used as a reference (HR=1). Compared with a lower cumulative time at an SBP of less than 100 mmHg, the risk for mortality increased for higher cumulative times. Furthermore, the risk for mortality tended to decrease with increased cumulative time at an SBP between 120 and 140 mmHg (Figure 3). This trend was not observed for the percentage of cumulative time at an SBP between 100 and 120 mmHg and 140 mmHg or more.
In our cox proportional hazards regression models, we observed an independent, graded relationship between the length of time spent with an SBP of less than 100 mmHg or SBP of 120-140 mmHg and in-hospital mortality (Table 2). Compared with patients at level 1, those with the most prolonged periods at an SBP of less than 100 mmHg had an approximately 4.24-fold increased risk of mortality. Furthermore, compared to patients with the lowest proportion of time spent with SBP 120-140 mmHg (Level 1), those with increasingly higher proportions of time within this range exhibited a stepwise decrease in mortality risk. The odds ratios (ORs) for mortality decreased from 0.62 (95% CI, 0.57-0.67) for Level 2 to 0.49 (95% CI, 0.42-0.56) for Level 4. Notably, the cumulative time spent within the SBP ranges of 100-120 mmHg and ≥140 mmHg did not emerge as independent predictors of mortality in the multivariate Cox regression analysis.
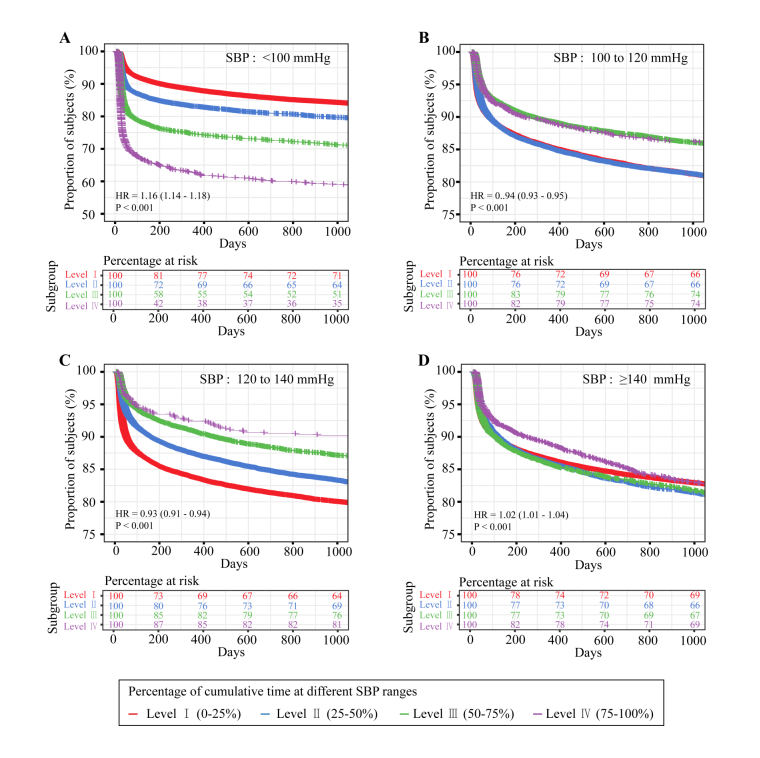
Figure 2. Kaplan-Meier survival curve of 1000-day mortality by the four levels of percentage of cumulative time at different systolic blood pressure levels in critically ill patients.
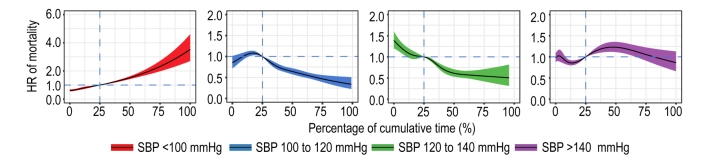
Figure 3. Hazard ratios 1-year mortality according to the percentage of cumulative time at different SBP ranges.
Table 2. Cox regression results regarding percentages of cumulative time at different systolic blood pressure levels.
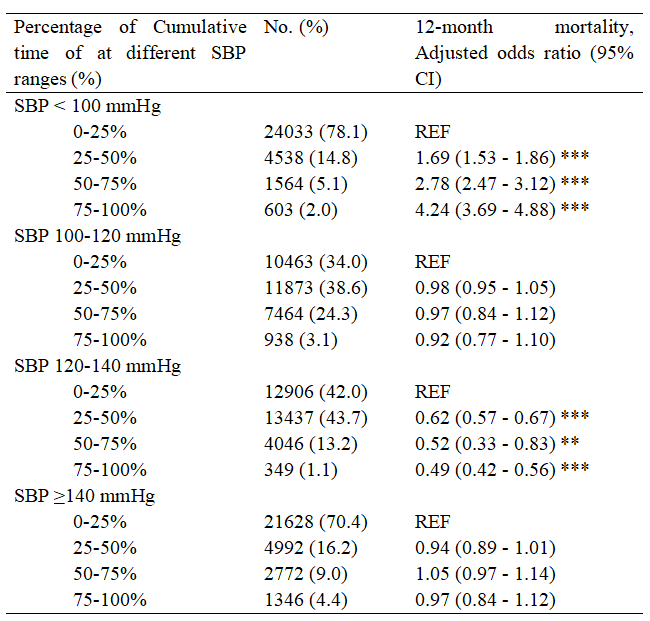
Abbreviation: CI, confidence interval; Ref, reference.
Cox model was adjusted for patient age, sexuality, ethnicity, types of admission, fluid volume intake and output, urine volume, minimum time of activated partial thromboplastin, minimum white blood cell count, minimum level of blood lactic acid, serum creatinine and total bilirubin, duration of mechanical ventilation and vasopressor usage.
*P<0.05, **P<0.01 and ***P<0.001.
Discussion
This study examined the relationship between the total duration of time spent at different systolic blood pressure levels and the outcomes of critically ill patients. Our findings indicate that a cumulative SBP below 100 mmHg is associated with increased mortality after ICU admission. Conversely, maintaining an SBP of 120-140 mmHg was linked to improved outcomes. Unlike static baseline characteristics, SBP can often be managed after ICU admission, making it a potential therapeutic target. Understanding this relationship could guide future interventions for critically ill patients.
Our study's unique strength lies in accounting for each minute spent with SBP below 100 mmHg, providing a sensitive assessment of SBP's impact on outcomes. We observed a rapid escalation of risk with no safe duration at this low SBP, emphasizing the importance of addressing hypotension due to its prevalence and association with morbidity (3,13,16).
While the optimal SBP level for critically ill patients remains unclear, our study offers insights into the clinically relevant degree and duration of time spent within specific SBP ranges. Notably, we found that maintaining an SBP between 120-140 mmHg was an independent protective factor in a diverse ICU patient cohort. This aligns with previous research demonstrating increased mortality associated with both hypotension and hypertension in the first 24 hours after out-of-hospital cardiac arrest (8), as well as in acute aortic dissection patients with SBP either ≤100 mmHg or >180 mmHg (16). Additionally, a secondary analysis of large trials found the lowest risk associated with an SBP of 120-140 mmHg in high cardiovascular risk patients (13).
Our study's strengths include the analysis of over 3.7 million SBP measurements from 30,738 critically ill patients, providing a comprehensive representation of hemodynamics and sufficient statistical power. Notably, our focus on a diverse ICU population distinguishes our study from others that examine specific patient groups or disease processes (4,13,16). However, our conclusions may not be generalizable to ICU populations with specific blood pressure targets (e.g., circulatory shock, aortic dissection), where active treatment of the underlying condition is paramount (15).
Although various statistical methods yielded consistent results, potential unmeasured confounders like ischemic cardiomyopathy could exist (5,17). Additionally, while we found an association between prolonged SBP within 120-140 mmHg and decreased mortality, this may be influenced by myocardial injury, which is prevalent but often underdiagnosed in ICU patients (18). Future research should explore this relationship further, potentially considering troponin monitoring.
Acknowledgments
We are grateful to the Laboratory of Computational Physiology at the Massachusetts Institute of Technology for providing the data used in this research.
Data availability
Data is available on request by emailing to Mr. Huo at huojian@szus.org
Contributors
According to the guidelines of the International Committee of Medical Journal Editors (ICMJE), all authors contributed to the four criteria. JBH and AMH conceived and designed the study. YS and MYX acquired the data. LY and AMH analyzed and interpreted the data. DQH and AMH drafted the manuscript. JH and AMH critically revised the manuscript for valuable intellectual content. All authors read and approved the final manuscript.
Conflicts of Interest:
The authors declare that they have no competing interests.
Funding
Dr. Zhang Xueping received funding from Shenzhen Municipal Science and Technology Fund (202205303002283).
Abbreviations
APACHE: acute physiology and chronic health evaluation
CAM-ICU: confusion assessment method for the intensive care unit
CCU: cardiac care unit
CI: confidence interval
DEX: dexmedetomidine
eICU: eICU collaborative research database
ERP: event related potential
GCS: Glasgow coma scale
Hb: hemoglobin
ICU: intensive care unit
MAP: mean atrial pressure
MBP: mean blood pressure
MICE: multivariate imputation by chain equations
MIMIC: multiparameter intelligent monitoring in intensive care
NICU: neurological intensive care unit
OR: odds ratio
PM: propensity matching
SICU: surgical intensive care unit
SMD: standard mean difference
vmPFC: ventromedial prefrontal cortex
WBC: white blood cell
References
- Schuurmans J, van Rossem BTB, Rellum SR, Tol JTM, Kurucz VC, van Mourik N, et al. Hypotension during intensive care stay and mortality and morbidity: a systematic review and meta-analysis. Intensive Care Med. 2024 Apr;50(4):516–25.
- Khanna AK, Maheshwari K, Mao G, Liu L, Perez-Protto SE, Chodavarapu P, et al. Association Between Mean Arterial Pressure and Acute Kidney Injury and a Composite of Myocardial Injury and Mortality in Postoperative Critically Ill Patients: A Retrospective Cohort Analysis. Crit Care Med. 2019 Jul;47(7):910–7.
- Maheshwari K, Nathanson BH, Munson SH, Khangulov V, Stevens M, Badani H, et al. The relationship between ICU hypotension and in-hospital mortality and morbidity in septic patients. Intensive Care Med. 2018 Jun;44(6):857–67.
- Ferreira JP, Duarte K, Pfeffer MA, McMurray JJV, Pitt B, Dickstein K, et al. Association between mean systolic and diastolic blood pressure throughout the follow-up and cardiovascular events in acute myocardial infarction patients with systolic dysfunction and/or heart failure: an analysis from the High-Risk Myocardial Infarction Database Initiative. Eur J Heart Fail. 2018 Feb;20(2):323–31.
- Andersson B, She L, Tan RS, Jeemon P, Mokrzycki K, Siepe M, et al. The association between blood pressure and long-term outcomes of patients with ischaemic cardiomyopathy with and without surgical revascularization: an analysis of the STICH trial. Eur Heart J. 2018 Oct 1;39(37):3464–71.
- Böhm M, Schumacher H, Teo KK, Lonn EM, Mahfoud F, Mann JFE, et al. Achieved blood pressure and cardiovascular outcomes in high-risk patients: results from ONTARGET and TRANSCEND trials. Lancet. 2017 Jun 3;389(10085):2226–37.
- Kalkman DN, Brouwer TF, Vehmeijer JT, Berger WR, Knops RE, de Winter RJ, et al. J Curve in Patients Randomly Assigned to Different Systolic Blood Pressure Targets: An Experimental Approach to an Observational Paradigm. Circulation. 2017 Dec 5;136(23):2220–9.
- McGuigan PJ, Giallongo E, Blackwood B, Doidge J, Harrison DA, Nichol AD, et al. The effect of blood pressure on mortality following out-of-hospital cardiac arrest: a retrospective cohort study of the United Kingdom Intensive Care National Audit and Research Centre database. Crit Care. 2023 Jan 5;27(1):4.
- Vincent JL, Nielsen ND, Shapiro NI, Gerbasi ME, Grossman A, Doroff R, et al. Mean arterial pressure and mortality in patients with distributive shock: a retrospective analysis of the MIMIC-III database. Ann Intensive Care. 2018 Nov 8;8(1):107.
- Kremer KM, Braisch U, Rothenbacher D, Denkinger M, Dallmeier D. Systolic Blood Pressure and Mortality in Community-Dwelling Older Adults: Frailty as an Effect Modifier. Hypertension. 2022 Jan;79(1):24–32.
- Cotter G, Metra M, Davison BA, Jondeau G, Cleland JGF, Bourge RC, et al. Systolic blood pressure reduction during the first 24 h in acute heart failure admission: friend or foe? Eur J Heart Fail. 2018 Feb;20(2):317–22.
- Vidal-Petiot E, Ford I, Greenlaw N, Ferrari R, Fox KM, Tardif JC, et al. Cardiovascular event rates and mortality according to achieved systolic and diastolic blood pressure in patients with stable coronary artery disease: an international cohort study. Lancet. 2016 Oct 29;388(10056):2142–52.
- Böhm M, Schumacher H, Teo KK, Lonn EM, Mahfoud F, Mann JFE, et al. Cardiovascular outcomes and achieved blood pressure in patients with and without diabetes at high cardiovascular risk. Eur Heart J. 2019 Jul 1;40(25):2032–43.
- Johnson AEW, Pollard TJ, Shen L, Lehman LWH, Feng M, Ghassemi M, et al. MIMIC-III, a freely accessible critical care database. Sci Data. 2016 May 24;3:160035.
- Asfar P, Meziani F, Hamel JF, Grelon F, Megarbane B, Anguel N, et al. High versus low blood-pressure target in patients with septic shock. N Engl J Med. 2014 Apr 24;370(17):1583–93.
- Havel C, Arrich J, Losert H, Gamper G, Müllner M, Herkner H. Vasopressors for hypotensive shock. Cochrane Database Syst Rev. 2011 May 11;(5):Cd003709.
- Vidal-Petiot E, Sorbets E, Bhatt DL, Ducrocq G, Elbez Y, Ferrari R, et al. Potential impact of the 2017 ACC/AHA guideline on high blood pressure in normotensive patients with stable coronary artery disease: insights from the CLARIFY registry. Eur Heart J. 2018 Nov 14;39(43):3855–63.
- Lim W, Qushmaq I, Cook DJ, Crowther MA, Heels-Ansdell D, Devereaux PJ. Elevated troponin and myocardial infarction in the intensive care unit: a prospective study. Crit Care. 2005;9(6):R636-44.
Share this Articles