Comparison of remazolam and propofol on the recovery of psychomotor function after painless gastrointestinal endoscopy
Shuang-yan Hu, MSMS1, Junfeng Hu, MSMS1, Lin-ling Mao, MSMS1, Yu-hong Zhao, MSMS1, Cheng Xu, MSMS1, Kai Qiu, MSMS1, Jun-feng Zhong, PhD1
1 Department of Anesthesiology, Shaoxing People's Hospital, Shaoxing People's Hospital, Shaoxing, China. *Corresponding authors at: 23 Tianbei 1st St, Wensheng Suite 1102, Shaoxing, 312000, China. E-mail addresses: junfzhong@qq.com (J. Zhong).
Abstract
Background: To enhance the outcomes for moderate to severe forms of Acute Respiratory Distress Syndrome (ARDS), a personalized lung-protective ventilation approach may be necessary. The challenge lies in personalizing medicine due to the heterogeneous nature of lung stress/strain.
Objective: To compare the recovery of psychomotor function after intravenous anesthesia with remimazolam or propofol combined with alfentanil in patients undergoing painless gastrointestinal endoscopy.
Methods: Seventy-eight patients undergoing painless gastrointestinal endoscopy were randomly divided into Group RA and Group PA. Remimazolam or propofol, in combination with alfentanil, was administered intravenously in Group RA or Group PA, respectively. Blood pressure, heart rate, respiratory rate, and oxygen saturation (SpO₂) were recorded before the procedure (T1), during the procedure (T2), upon awakening from anesthesia (T3), and at discharge from the PACU (T4). Psychomotor function was evaluated using the Trieger Dot Test (TDT) and the Digit Symbol Substitution Test (DSST) at T1, T4, 1 hour post-procedure (T5), and 2 hours post-procedure (T6).
Results: Assessment of the TDT showed that the number of dots missed (NDM), the maximum distance of dots missed (MDDM), and the average distance of dots missed (ADDM) at T4 and T5 were significantly lower than at T1 in both groups. The completion rates and accuracy rates of the DSST at T4 and T5 were significantly lower than at T1. However, results of the TDT and DSST at T6 were not significantly different from those at T1. At T4 and T5, the NDM, MDDM, and ADDM values in Group RA were significantly lower than those in Group PA. The completion and accuracy rates of the DSST at T4 and T5 in Group RA were significantly higher compared to Group PA. Additionally, the incidence of hypotension was significantly lower in Group RA compared to Group PA, while there was no significant difference in the incidence of respiratory depression between the groups.
Conclusions: Psychomotor function fully recovered within 2 hours after surgery when remimazolam combined with alfentanil was used for painless gastrointestinal endoscopy. Compared to propofol, psychomotor function recovery in the remimazolam group was faster, with fewer adverse effects observed post-surgery.
Trial registration: Not applicable.
Keywords: Remimazolam; Alfentanil; Propofol; Gastrointestinal Endoscopy; Psychomotor Function
Introduction
After intravenous painless anesthesia with propofol, patients experience impaired psychomotor function postoperatively, which affects activities such as driving or riding in vehicles, cycling, and operating machinery [1-3]. Currently, there is ongoing debate regarding when patients can resume normal activities and driving after painless anesthesia. Clinicians generally advise against driving or traveling alone within 24 hours after undergoing painless procedures.
Remimazolam, a novel water-soluble, ultra-short-acting anesthetic sedative, causes no injection pain and has minimal effects on respiration and hemodynamics, making it more suitable for painless endoscopic anesthesia [4-6]. Animal studies have shown that remimazolam affects cognitive function in elderly rats [7], and clinical research on its postoperative effects on cognition and psychomotor function has yielded inconsistent results [8-9].
The effects of propofol on tasks such as the digit symbol substitution test and simulated driving ability can last for 1–2 hours after administration [1,8]. However, there is limited research on the recovery of psychomotor function in patients following intravenous anesthesia with remimazolam for painless endoscopy. This study aims to compare the recovery of psychomotor function in patients undergoing painless gastrointestinal endoscopy anesthesia with remimazolam versus propofol.
Methods
Clinical Data
This study was approved by the hospital's ethics committee (Ethics Approval No. 038/2023). Patients and their families were informed about the study and voluntarily signed informed consent forms.
The inclusion criteria were as follows: inpatients undergoing painless gastrointestinal endoscopy, age >18 years, BMI of 18–30 kg/m², and ASA classification of I or II. Patients were excluded if they had allergies to benzodiazepines, propofol, or opioids; preoperative assessment indicating a difficult airway (Mallampati grade >III) or sleep apnea; long-term use of sedatives or hypnotics; severe cardiovascular or cerebrovascular diseases, significant cardiac conduction block, severe hepatic or renal insufficiency, or neurological or psychiatric disorders. Pregnant women or those planning to conceive soon, as well as patients with other conditions deemed unsuitable for the study, were also excluded.
A total of 78 patients were enrolled and randomly assigned using a random number table into two groups: the remimazolam with alfentanil group (RA group, n=39) and the propofol with alfentanil group (PA group, n=39).
Preoperative Preparation
After entering the examination room, patients were positioned in the left lateral decubitus position. Peripheral venous access was established in the upper limb, and lactated Ringer's solution was infused intravenously. Five minutes before the procedure, all patients orally administered 10 mL of lidocaine gel for oropharyngeal surface anesthesia. Nasal oxygen was provided at 4 L/min, and continuous monitoring of blood pressure (BP), heart rate (HR), respiratory rate (RR), and oxygen saturation (SpO₂) was performed.
Anesthetic Protocol
Both groups received an intravenous injection of alfentanil (Batch No. 23S10021, Yichang Humanwell Pharmaceutical Co., Ltd.) at a dose of 4 μg/kg. After one minute, the RA group received a slow intravenous injection of remimazolam (Batch No. 20T05081, Yichang Humanwell Pharmaceutical Co., Ltd.) at 0.2 mg/kg, while the PA group received propofol (Batch No. 12211212, Xi'an Janssen Pharmaceutical Co., Ltd.) at 1.5–2.0 mg/kg.
Gastrointestinal endoscopy began when the patient achieved an OAA/S sedation score ≤2. During the procedure, if HR increased by more than 15% of baseline or exceeded 90 bpm, SBP rose by more than 15% of baseline, or coughing or movement occurred, the RA group received additional remimazolam (0.05 mg/kg), and the PA group received additional propofol (0.5 mg/kg) until the OAA/S score was ≤2.
Respiratory depression was defined as SpO₂ <90% for more than 10 seconds. In such cases, oxygen flow was increased, and pure oxygen was administered via a mask if necessary. SBP <80 mmHg or a reduction >30% of baseline was treated with ephedrine (5–10 mg), while HR <45 bpm was treated with atropine (0.5 mg per dose). After the procedure, all patients were transferred to the PACU for recovery. Awakening was assessed using the modified Aldrete score, and patients were discharged from the PACU when their score was ≥9, accompanied by a family member.
Monitoring Indicators
The study compared the following parameters between the two groups: the total anesthetic dosage, frequency of additional remimazolam or propofol administration, eye-opening time (from the last dose to eye opening upon command), and recovery time (from the last dose to a modified Aldrete score greater or equal than 9). BP, HR, RR, and SpO₂ were recorded at four time points: preoperative baseline (T1), start of the procedure (T2), awakening (T3), and discharge from PACU (T4).
Psychomotor function was assessed using the Trieger dot test (TDT) and the digit symbol substitution test (DSST) at T1, T4, one hour post-procedure (T5), and two hours post-procedure (T6). The TDT required patients to connect 42 dots into two intersecting S-shaped curves, and the DSST involved matching symbols to 125 numbers (1–9) within 120 seconds. The following were recorded: for the TDT, the number of dots missed (NDM), maximum distance of dots missed (MDDM), and average distance of dots missed (ADDM); for the DSST, the completion rate and accuracy rate at each time point.
These tests were administered under the guidance of blinded anesthesiologists.
Statistical Methods
Data were analyzed using SPSS 25.0 software. Normally distributed continuous data were expressed as mean ± standard deviation (x̄ ± s) and compared between groups using independent sample t-tests. Repeated measures ANOVA was used to compare intra-group changes over time. Categorical data were compared using the χ² test or Fisher's exact test. A P value <0.05 was considered statistically significant.
Table 1. Comparison of general information between the two groups (x̄±s, n=39)
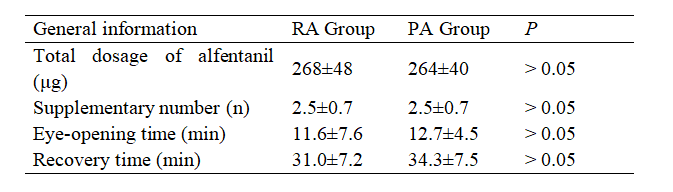
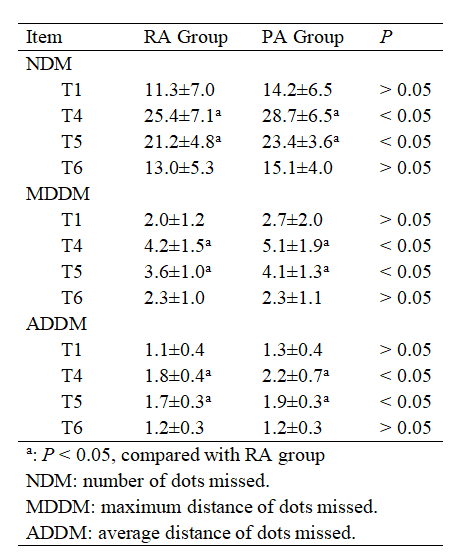
Table 2. Comparisonof NDM, MDDM, ADDM in Tridger test at different time in two groups
Results
There were no statistically significant differences between the two groups in terms of age, gender, BMI, education level, ASA classification, total dosage of alfentanil, number of supplementary doses of remimazolam or propofol, eye-opening time, and recovery time (P > 0.05), as shown in Table 1.
At T2, T3, and T4, the SBP, DBP, and HR of the PA group were significantly lower than those of the RA group, with differences being statistically significant (P < 0.05). There were no statistically significant differences between the groups for RR at all time points (P > 0.05). Compared with T1, both groups showed significant reductions in SBP, DBP, and RR at T2 (P < 0.05), but there were no significant differences in HR (P > 0.05). Compared with T1, there were no significant reductions in SBP, DBP, HR, and RR at T3 and T4, with no statistically significant differences (P > 0.05).
Compared with T1, both groups showed an increase in NDM, MDDM, and ADDM at T4 and T5, with statistically significant differences (P < 0.05). There were no statistically significant differences at T6 (P > 0.05). Between the two groups, the RA group had lower NDM, MDDM, and ADDM values than the PA group at T4 and T5, with statistically significant differences (P < 0.05). At T6, there were no significant differences between the two groups (P > 0.05). The results are shown in Table 2.
Table 3. Comparison of DSST results at different time points between the two groups
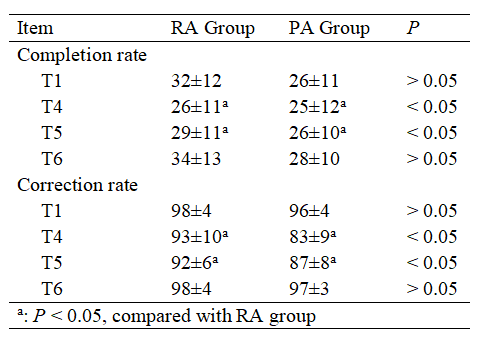
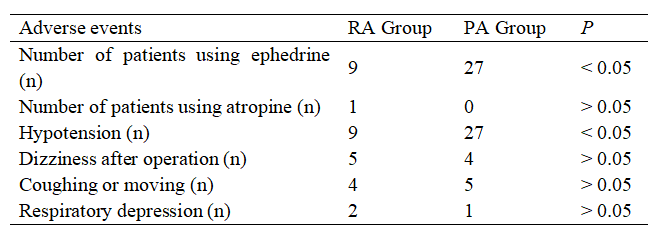
Table 4. Comparison of adverse events between the two groups
Compared with T1, the completion rate and accuracy of DSST were lower at T4 and T5 in both groups, with statistically significant differences (P<0.05). There were no statistically significant differences at T6 (P > 0.05). When comparing between the two groups, the RA group had higher completion rates and accuracy than the PA group at T4 and T5, with statistically significant differences (P < 0.05). At T6, there were no significant differences between the groups (P > 0.05). The results are shown in Table 3.
The incidence of intraoperative hypotension and the use of ephedrine were lower in the RA group than in the PA group, with statistically significant differences (P < 0.05). There were no statistically significant differences between the groups in the use of atropine, incidence of coughing/movement, respiratory depression, and postoperative dizziness (P > 0.05), as shown in Table 4.
Discussion
This study used two methods, TDT and DSST, to comprehensively evaluate the recovery of psychomotor function after painless gastrointestinal endoscopy. The results showed that in patients receiving remimazolam combined with alfentanil intravenous anesthesia, the TDT and DSST scores at 1 hour after surgery were still lower than preoperative values, but recovered completely at 2 hours postoperatively. Compared to propofol, remimazolam resulted in more complete recovery of psychomotor function within 1 hour after anesthesia.
Propofol is a commonly used anesthetic for painless gastrointestinal endoscopy. The impact of intravenous propofol anesthesia on patients' digital symbol substitution test (DSST) and simulated driving ability lasts for 1-2 hours after administration [1,10], with older patients experiencing delayed recovery of psychomotor function [11]. Grant et al. suggested that a propofol blood concentration of 200 ng/mL is equivalent to a blood alcohol concentration of 20 ng/mL, which is much lower than the legal standard for driving under the influence (80 ng/mL) [12]. Studies also show that after 1 hour of intravenous propofol anesthesia (200 mg), 97.7% of patients have a propofol blood concentration ≤200 ng/mL [1]. Therefore, the current regulation that patients must wait 24 hours after propofol anesthesia before returning to work or driving seems overly strict.
With the increasing use of alfentanil combined with propofol in painless gastrointestinal endoscopy anesthesia, alfentanil has significantly reduced the amount of propofol required, decreasing the incidence of hypotension, respiratory depression, coughing, and body movement [13-14]. Although alfentanil combined with propofol also affects postoperative psychomotor function recovery [15], whether it is necessary to restrict patients from driving within 24 hours postoperatively is still open for discussion. Doganay et al. observed that, in patients undergoing painless colonoscopy with alfentanil and propofol, cognitive function was less affected within 30 minutes postoperatively compared to fentanyl, but they did not clarify whether cognitive function was completely restored at 30 minutes [16]. Most studies have only compared the differences in psychomotor or cognitive function between different drug combinations. This study not only analyzed the recovery of psychomotor function in patients after anesthesia with two drug combinations but also compared psychomotor function at different time points within each group to pre-anesthesia baseline values. The results showed that psychomotor function in both groups fully recovered to pre-examination levels at 2 hours postoperatively. Therefore, the results of this study provide a reference for when painless anesthesia patients can resume normal daily activities postoperatively.
Remimazolam is a new ultra-short-acting benzodiazepine sedative, an ideal drug for painless anesthesia. When combined with alfentanil or sufentanil, it achieves good effects in painless anesthesia [4-5]. Remimazolam has been shown to upregulate the expression of ApoE and Tau proteins in the hippocampus of aged rats, which is related to cognitive dysfunction. However, clinical studies on the effects of remimazolam on postoperative cognitive and psychomotor function are inconsistent. Choil et al. compared continuous infusion of remimazolam with target-controlled infusion of propofol in women undergoing thyroid surgery and found no significant difference in the quality of recovery (QoR-15) scores at 1 and 2 days postoperatively [9]. Takahito et al. compared the recovery of psychomotor function after anesthesia with remimazolam and propofol in patients undergoing general anesthesia with intubation and found that remimazolam had a significantly greater impact on psychomotor function between 30 minutes and 2 hours postoperatively, though this group of patients woke up faster [8]. Both of these studies involved patients undergoing general anesthesia with intubation, where the recovery of psychomotor function might be influenced by factors such as intraoperative anesthesia and surgical methods. Remimazolam, however, is more suitable for outpatient painless examinations and day surgeries. Therefore, studying the recovery of psychomotor function in patients after painless anesthesia has important clinical significance.
In this study, propofol, a classic drug for painless anesthesia, was used as a control. The results showed that the time for complete recovery of psychomotor function in the remimazolam group was similar to the propofol group (2 hours postoperatively). However, within 1 hour after surgery, the NDM, MDDM, and ADDM scores were significantly lower in the remimazolam group than in the propofol group, and the DSST completion rate and accuracy were significantly higher in the remimazolam group. This suggests that remimazolam has an effect on postoperative cognitive function, but its impact on early postoperative psychomotor function is less than that of propofol, indicating that patients receiving remimazolam anesthesia have a more complete recovery of psychomotor function within 1 hour postoperatively. The results of this study are inconsistent with those of Choil and Takahito, which may be due to differences in drug administration methods, dosages, surgical approaches, and observation times. The recovery of psychomotor function in patients after remimazolam anesthesia still requires further clinical research to confirm.
Propofol can reduce airway reactivity, potentially leading to respiratory arrest and myocardial suppression. In painless gastrointestinal endoscopy, 90% of patients who experience cardiac arrest are caused by propofol. On the other hand, the likelihood of respiratory depression with remimazolam is minimal, with an incidence of hypotension and hypoxemia at only 1%. Therefore, remimazolam has potential advantages in painless endoscopy [17]. The results of this study show that remimazolam has less impact on intraoperative circulation, and its effects on respiratory depression and recovery time are similar to those of propofol, with no increased incidence of intraoperative body movement or coughing.
TDT is a reliable method for evaluating the recovery of psychomotor function after anesthesia [16,18]. DSST is a commonly used method to assess patients' neurocognitive function by observing attention, visual perception, and motor efficiency [19-20]. Considering that the evaluation of TDT and DSST may be influenced by factors such as education level, age, and depth of anesthesia, we divided education level into three categories for analysis. The results showed no significant difference between the two groups in education level and age. A limitation of this study is that objective indicators of anesthesia depth (such as BIS) were not used during the examination process, and sedation was assessed based on the OAA/S scale, which may have influenced the results.
In conclusion, intravenous anesthesia with remimazolam combined with alfentanil is safe for painless gastrointestinal endoscopy. After painless gastrointestinal endoscopy with either remimazolam or propofol, patients' psychomotor function is fully restored within 2 hours postoperatively. However, recovery is faster in the remimazolam group, with fewer adverse reactions.
Data sharing statement
Patient data is not available due to sensitivity reasons.
Contributors
According to the guidelines of the International Committee of Medical Journal Editors (ICMJE), all authors contributed to the four criteria. SYH and JFZ conceived and designed the study. JFH, YHZ and LLM acquired the data. CX and KQ analyzed and interpreted the data. SYH and LLM drafted the manuscript. JFH and JFZ critically revised the manuscript for valuable intellectual content. All authors read and approved the final manuscript.
Conflicts of Interest:
The authors declare that they have no competing interests.
Abbreviations
ADDM: average distance of dots missed
ASA: American society of anesthesiologists
BP: blood pressure
DBP: diastolic blood pressure
DSST: digit symbol substitution test
HR: heart rate
MDDM: maximum distance of dots missed
NDM: number of dots missed
OAA/Ss: observer’s assessment of alertness/sedation
PACU: post-anesthesia care unit
RR: respiratory rate
SBP: systolic blood pressure
SP0₂: peripheral oxygen saturation
TDT: trieger dot test
References
- Horiuchi A, Nakayama Y, Fujii H, et al. Psychomotor recovery and blood propofol level in colonoscopy when using propofol sedation [J]. Gastrointest Endosc, 2012, 75(3): 506-512.
- Riphaus A, Gstettenbauer T, Frenz MB, et al. Quality of psychomotor recovery after propofol sedation for routine endoscopy: a randomized and controlled study [J]. Endoscopy, 2006, 38(7): 677-683.
- Willey J, Vargo JJ, Connor JT, et al. Quantitative assessment of psychomotor recovery after sedation and analgesia for outpatient EGD [J]. Gastrointest Endosc, 2002, 56(6): 810-816.
- Xu Chang, He Long, Ren Juanjuan, et al. Evaluation of anesthesia effect in painless gastroscopy using remimazolam combined with alfentanil [J]. Chinese Journal of Anesthesiology, 2022, 42(10): 1215-1218.
- Wei Hua, Zhang Le, Li Lu. Effect of remimazolam combined with alfentanil for frail elderly patients undergoing gastroscopy [J]. Chinese Journal of Anesthesiology, 2022, 42(6): 708-711.
- Luo Kai, Fu Huangde, Yao Jiemin. Research progress in the clinical application of remimazolam [J]. Chinese Journal of Intensive Care Medicine Electronic Edition, 2021, 7(1): 71-75.
- Shi Yuan, Jiang Yi, Dong Beibei, et al. A comparison of the effects of remimazolam and midazolam on cognitive function in healthy aging rats [J]. Chinese Journal of Anesthesiology, 2020, 40(9): 1089-1092.
- Shimizu T, Takasusuki T, Yamaguchi S. Remimazolam compared to propofol for total intravenous anesthesia with remifentanil on the recovery of psychomotor function: A randomized controlled trial [J]. Adv Ther, 2023, 40(10): 4395-4404.
- Choi JY, Lee HS, Kim JY, et al. Comparison of remimazolam-based and propofol-based total intravenous anesthesia on postoperative quality of recovery: A randomized non-inferiority trial [J]. J Clin Anesth, 2022, 82: 110955.
- Sinclair DR, Chung F, Smiley A. General anesthesia does not impair simulator driving skills in volunteers in the immediate recovery period—a pilot study [J]. Can J Anaesth, 2003, 50(3): 238-245.
- Shinozaki M, Usui Y, Yamaguchi S, et al. Recovery of psychomotor function after propofol sedation is prolonged in the elderly [J]. Can J Anaesth, 2002, 49(9): 927-931.
- Grant SA, Murdoch J, Millar K, et al. Blood propofol concentration and psychomotor effects on driving skills [J]. Br J Anaesth, 2000, 85(3): 396-400.
- Wang LL, Guan ZY, Wang CM, et al. A comparative study on the efficacy and safety of propofol combined with different doses of alfentanil in gastroscopy: a randomized controlled trial [J]. J Anesth, 2023, 37(2): 201-209.
- Yang H, Shi X, Li J, et al. Efficacy and safety of alfentanil plus propofol versus propofol only in painless gastrointestinal endoscopy: A meta-analysis [J]. Medicine (Baltimore), 2023, 102(32): e34745.
- Zhu X, Chen X, Zheng X, et al. Effects of single-use alfentanil versus propofol on cognitive functions after colonoscopy: A randomized controlled trial [J]. Heliyon, 2023, 9(6): e17061.
- Doganay G, Ekmekci P, Kazbek BK, et al. Effects of alfentanil or fentanyl added to propofol for sedation in colonoscopy on cognitive functions: Randomized controlled trial [J]. Turk J Gastroenterol, 2017, 28(6): 453-459.
- Rex DK, Bhandari R, Desta T, et al. A phase III study evaluating the efficacy and safety of remimazolam (CNS7056) compared with placebo and midazolam in patients undergoing colonoscopy [J]. Gastrointest Endosc, 2018, 88(3): 427-437.
- Mishra SK, Chandrasekaran A, Parida S, et al. Time course of psychomotor recovery after intravenous dexmedetomidine infusion as a part of balanced anesthetic technique: A randomized, double-blind study [J]. Indian J Anaesth, 2019, 63(8): 623-628.
- Williamson M, Maruff P, Schembri A, et al. Validation of a digit symbol substitution test for use in supervised and unsupervised assessment in mild Alzheimer's disease [J]. J Clin Exp Neuropsychol, 2022, 44(10): 768-779.
- Jaeger J. Digit symbol substitution test: The case for sensitivity over specificity in neuropsychological testing [J]. J Clin Psychopharmacol, 2018, 38(5): 513-519.
Share this Articles