Effect of dexmedetomidine on hemodynamics in abdominal surgery patients undergoing intravenous-inhalation combined general anesthesia
Ying Xu, MD¹, Ying-jie Jin, PhD²*
¹ Department of Anesthesiology, Suzhou Yongding Hospital, Suzhou, China. ² Department of Anesthesiology, Jiangsu Shengze Hospital Affiliated to Nanjing Medical University, Nanjing, China. *Corresponding authors at: No. 1399, Market West Road, Shengze Town, Wujiang District, Jiangsu, 210000, China. E-mail addresses: Yjiejin@qq.com (Y. Jin).
Abstract
Background: Abdominal surgery is a common surgical procedure with a wide range of applications in treating various diseases. Anesthetic protocol and drug selection significantly influence surgical outcomes in abdominal procedures. Dexmedetomidine is widely used as an efficient adjunct in surgical anesthesia, however its effect on patients’ hemodynamics in abdominal surgery is poorly investigated.
Objective: To investigate the effects of dexmedetomidine on hemodynamics in patients undergoing abdominal surgery with intravenous-inhalation combined general anesthesia.
Methods: A total of 100 patients scheduled for major elective abdominal surgery at Suzhou Yongding Hospital from January 2021 to February 2024 were selected. Using a random number table, patients were divided into a control group and a study group, each with 50 patients. The control group received inhalational anesthesia with sevoflurane in combination with opioid analgesics and muscle relaxants. The study group received an intravenous infusion of dexmedetomidine at 0.8 μg/(kg·h) at the start of surgery, along with inhalation of sevoflurane at 0.8 minimum alveolar concentration, combined with opioid analgesics and non-depolarizing muscle relaxants. Surgical indicators, Visual Analogue Scale (VAS) pain scores, and incidence of adverse events were compared between the groups.
Results: Both groups successfully completed anesthesia and surgery. Compared to the control group, the study group experienced less intraoperative circulatory fluctuation, resulting in more stable vital signs. There was no significant difference between the two groups in terms of surgical duration, recovery time, resting VAS pain score at 1 hour postoperatively, or incidence of nausea and vomiting (P > 0.05). The study group’s mean arterial pressure (MAP) remained stable at various time points, whereas the control group exhibited greater variability in MAP. The MAP values at T1-T4 were significantly different between the groups (P < 0.05).
Trial registration: Not applicable.
Keywords: Abdominal surgery; General anesthesia; Dexmedetomidine; Adverse events; Hemodynamics
Introduction
Abdominal surgery is a frequently performed procedure with essential roles in diagnosing and treating a variety of diseases, including gastrointestinal, hepatic, and vascular conditions (1). Due to the complexities associated with abdominal surgeries, the choice of anesthetic protocol and drug selection is crucial, as they can substantially impact hemodynamic stability, pain management, recovery times, and overall patient outcomes (2). Dexmedetomidine, a selective α2-adrenergic receptor agonist, is particularly valued in these procedures; as an active dextrorotatory isomer of medetomidine, it offers targeted effects by effectively suppressing neuronal excitability, reducing sympathetic activity, and inhibiting norepinephrine release (3). These actions contribute to improved cardiovascular stability, decreased anesthetic requirements, and enhanced patient comfort.
Dexmedetomidine is thus widely utilized as an adjunct in surgical anesthesia, providing effective sedation, anxiolysis, and analgesia without significant respiratory depression. Its pharmacological benefits, including its neuroprotective and anti-inflammatory properties, make it an excellent choice for complex surgeries, helping to minimize postoperative complications and enhance recovery quality in patients undergoing abdominal procedures. This study explores the impact of different anesthesia adjuncts on hemodynamics in patients undergoing intravenous-inhalation combined general anesthesia for abdominal surgery.
Methods
General Information
A total of 100 patients scheduled for major elective abdominal surgery at Suzhou Yongding Hospital from January 2021 to February 2024 were selected. Using random assignments, patients were divided into a control group and a study group, each containing 50 patients. The groups had no significant differences in baseline characteristics (P > 0.05).
Inclusion and Exclusion Criteria
Inclusion criteria: 1. Patients with a pathological diagnosis of gastrointestinal or hepatopancreaticobiliary malignancies scheduled for radical open surgery. 2. Normal cardiac function or NYHA Class I-II (4), or ASA Class I-III (5), with BMI of 16-33 kg/m². 3. No allergies to the drugs used in the study. 4. No serious organ disease or blood or immune disorders. Exclusion criteria: 1. Blood pressure >= 170/100 mmHg or < 90/60 mmHg before surgery. 2. History of myocardial infarction, liver or kidney failure, severe respiratory or neurological disease within the past 3 months. 3. Allergy to the study drugs.
Interventions
Both groups underwent a standard fasting protocol, abstaining from food and drink for 6 to 8 hours before surgery. Thirty minutes before the operation, patients were administered 0.5 mg of atropine and 10 mg of diazepam via intramuscular injection. After entering the operating room, intravenous access was established.
For control group, anesthesia was induced using sevoflurane inhalation combined with opioid analgesics and muscle relaxants. While in study group, dexmedetomidine (produced by Jiangsu Enhua Pharmaceutical, registration number 20150102) was administered intravenously at 0.8 μg/(kg·h) at the start of surgery, along with sevoflurane at 0.8 MAC, in combination with opioid analgesics and non-depolarizing muscle relaxants to complete the anesthesia. A multi-functional anesthesia monitoring machine and a bispectral index (BIS) monitor were used to continuously monitor the patient’s BIS, heart rate (HR), oxygen saturation (SpO₂), mean arterial pressure (MAP), and respiratory rate (RR) in real time.
Outcome measuements
- Surgical Indicators: Duration, recovery time, time to respiration recovery, eye-opening, and extubation time.
- VAS Pain Score: Pain was assessed postoperatively on a 0-10 scale, with higher scores indicating greater pain severity (6).
- Adverse Events: Including coughing, agitation, nausea, vomiting, and sinus bradycardia.
- Hemodynamics: MAP was observed at pre-anesthesia (T0), 10 min after dexmedetomidine infusion (T1).
- min post-intubation (T2), at extubation (T3), and 5 min post-extubation (T4) (7).
SPSS 21.0 was used for statistical analysis, with χ² and t-tests.
Statistical analysis
All statistical analysis were performed using SPSS 21.0
Results
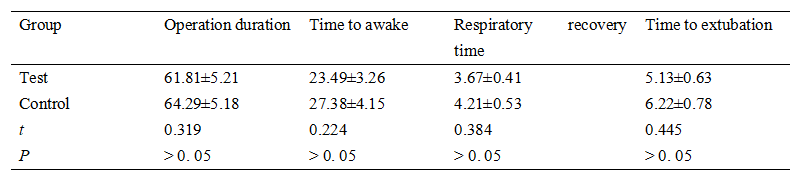
No significant difference in surgery related parameters was observed between the two groups (P > 0.05) as presented in Table 1.
Table 1. Clinical and demographic properties of the study population.
At 1 hour postoperatively at rest, there was no statistically significant difference in VAS scores between the two groups (1.32 ± 0.27) vs. (1.59 ± 0.31), t = 0.591, P > 0.05. However, at 4 hours postoperatively at rest, the VAS score in the study group (1.48 ± 0.15) was significantly lower than that in the control group (2.69 ± 0.62), with a statistically significant difference (t = 9.381, P < 0.05). As shown in table 2, there was no significant difference in the incidence of nausea and vomiting. However, the study group had a significantly lower overall adverse event rate (P < 0.05).
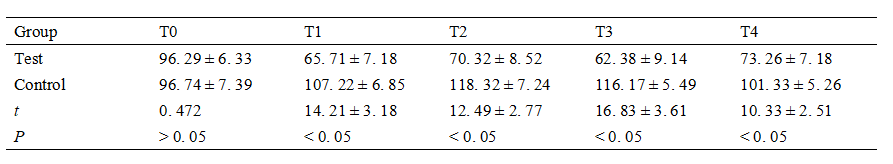
The study group’s MAP remained stable throughout the perioperative period, while the control group exhibited greater fluctuations in MAP, with significant differences at T1-T4 (P < 0.05). Hemodynamic outcomes were shown in table 3.
Table 2. Clinical and demographic properties of the study population.
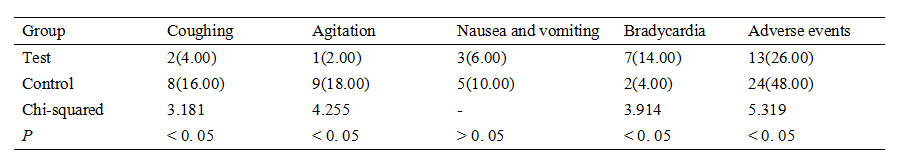
Table 3. Clinical and demographic properties of the study population.
Discussion
Current abdominal surgeries primarily employ two anesthetic pathways: inhalation anesthesia combined with total intravenous anesthesia (TIVA) and epidural anesthesia (8). According to relevant medical research, both inhalation anesthesia and epidural anesthesia can induce varying degrees of stress responses in patients during the perioperative period. The main clinical manifestations include abnormal sympathetic nervous system excitation, increased heart rate, elevated blood pressure, hyperglycemia, increased myocardial oxygen consumption, hemodynamic abnormalities, and external signs such as nausea, coughing, vomiting, and agitation. The occurrence of stress responses increases the risk of surgical procedures, significantly impacts the efficacy of surgical treatment (9), and can even pose a threat to patients' health and life. Therefore, the use of stress response inhibitors during anesthesia is crucial and necessary in abdominal surgeries.
Dexmedetomidine, a highly selective α2-adrenergic receptor agonist, has been widely used in clinical anesthesia due to its sedative, analgesic, and anti-sympathetic effects. It does not cause significant respiratory depression, making it an important adjunct to anesthesia for abdominal surgery. Dexmedetomidine can effectively reduce the incidence of various perioperative stress responses and help maintain stable hemodynamics in patients (11). Its application is particularly effective in abdominal surgeries using inhalation anesthesia combined with TIVA. The results of this study are consistent with those of Hu Rui (12), indicating that both anesthetic methods have good anesthetic effects, but dexmedetomidine can make patients' hemodynamics more stable and improve their perioperative comfort.
The reason is that dexmedetomidine has stronger analgesic, sedative, and anti-sympathetic effects compared to metomidine. As a highly selective central α2-adrenergic receptor agonist, its affinity for α2-adrenergic receptors is more than seven times that of clonidine (13). The primary pharmacological action of dexmedetomidine is to intervene in the α2A receptor subtype, thereby achieving therapeutic effects. The α2A receptor is located pre-synaptically and post-synaptically, and one of its important functions is to reduce the synthesis and secretion of norepinephrine in the human body and inhibit the excitation of neurons.
Dexmedetomidine can also stimulate and activate the pre-synaptic membrane α2 receptor, thereby inhibiting the synthesis and secretion of norepinephrine in the human body, and thus blocking and reducing the transmission of pain signals (14). Furthermore, it can activate the post-synaptic membrane receptor, effectively reducing sympathetic nerve activity and thus lowering heart rate and blood pressure.
Dexmedetomidine can also bind to α2 receptors in the human spinal cord, producing analgesic effects. Simultaneously, dexmedetomidine also has sedative and anxiolytic pharmacological effects. Therefore, the use of dexmedetomidine in abdominal surgery has multiple effects, and the rational use of dexmedetomidine dosage can effectively reduce the total amount of anesthetic drugs used in abdominal surgery, thereby effectively improving the safety of abdominal surgery and reducing adverse drug reactions caused by improper or excessive use of anesthetic drugs. Dexmedetomidine can also maintain stable hemodynamics in patients during surgery, effectively reducing the incidence of local myocardial ischemia in the surgical area.
Dexmedetomidine also has a pharmacological characteristic: its main component has a short half-life, with a distribution half-life of 6 minutes and an elimination half-life of 2 hours. Its pharmacokinetics is relatively strong, and it is the only drug among similar anesthetic drugs that combines sedative and analgesic effects.
Therefore, dexmedetomidine is a commonly used and highly effective adjunctive anesthetic drug for surgical anesthesia, both domestically and internationally, and has excellent pharmacological effects (15). The use of dexmedetomidine in surgical procedures can effectively reduce the dosage of other anesthetic drugs, thereby improving patient safety during surgery and reducing the incidence of anesthetic drug-related complications and adverse reactions. For example, remifentanil is a commonly used anesthetic drug for surgical anesthesia and has a wide and important application in inhalation anesthesia combined with TIVA for abdominal surgery. However, excessive use of remifentanil can cause adverse reactions in patients and produce related complications. The use of dexmedetomidine can effectively reduce the dosage of remifentanil, effectively increasing the pain threshold in patients during surgery. It can also significantly reduce the effect-site concentration of target-controlled infusion propofol, effectively reducing the dosage of propofol, and can also significantly reduce the dosage of postoperative analgesics such as morphine. Furthermore, the scientific use of dexmedetomidine dosage can effectively reduce patients' eye opening time and shorten the time for extubation, significantly improving patients' sedation and analgesia comfort during the perioperative period.
In conclusion, in the general anesthesia scheme for major abdominal surgery, inhalation anesthesia combined with TIVA with dexmedetomidine results in more stable hemodynamics during surgery and a lower incidence of cardiovascular adverse events.
Data sharing statement
Patient data is not available due to sensitivity reasons
Contributors
According to the guidelines of the International Committee of Medical Journal Editors (ICMJE), all authors contributed to the four criteria. YJJ conceived and designed the study. YX acquired the data. YX and YJJ analyzed and interpreted the data. YX drafted the manuscript. YJJ critically revised the manuscript for valuable intellectual content. All authors read and approved the final manuscript.
Conflicts of Interest:
The authors declare that they have no competing interests.
Abbreviations
ASA: American society of anesthesiologists
BMI: body mass index
NYHA: New York heart association
TIVA: total intravenous anesthesia
VAS: visual analogue scale
References
- Zhang ZJ, Liu LM, Huang WB, et al. Application of dexmedetomidine hydrochloride combined with ultrasound-guided femoral nerve and lateral femoral cutaneous nerve block and inhalation anesthesia in elderly patients with femoral fracture surgery. Chinese Journal of Disability Medicine, 2023, 31(18): 162-165.
- Guan X, Ma BX, Song MG, et al. Effect of lumbar plexus-sacral plexus nerve block combined with dexmedetomidine under ultrasound and nerve stimulator guidance on elderly patients undergoing femoral proximal anti-rotation intramedullary nail surgery. Modern Medicine and Health Research Electronic Journal, 2022, 6(1): 4-7.
- Li XJ. Effect of dexmedetomidine combined with ropivacaine in ultrasound-guided brachial plexus block analgesia. Jilin Medicine, 2023, 44(10): 2888-2891.
- Jiang X, Tang X, Liu S, et al. Effects of dexmedetomidine on evoked potentials in spinal surgery under combined intravenous inhalation anesthesia: a randomized controlled trial. BMC Anesthesiol, 2023, 23(1): 36.
- Qiu YQ, Zhang LP, Wu PY, et al. Effect of dexmedetomidine on postoperative renal function in patients undergoing cardiac valve surgery under cardiopulmonary bypass: a randomized clinical trial. J Cardiothorac Vasc Anesth, 2023, 37(8): 1424-1432.
- Pang CG, Zeng QL, Xu YX, et al. Effect of continuous intravenous infusion of dexmedetomidine combined with inhalation anesthesia on patients undergoing extracorporeal circulation heart valve replacement surgery. Chinese Science and Technology Journal Database Medicine, 2022, 19(2): 475-478.
- Lu Y. Effect of low-dose dexmedetomidine combined with general anesthesia on hemodynamic disturbance and perioperative cardiac adverse events in patients with high cardiovascular risk undergoing elective lower abdominal surgery. Chinese Medical Innovation, 2022, 19(4): 145-149.
- Tong CT, Yang L, Li HX. Effect of dexmedetomidine combined with parecoxib on recovery quality and hemodynamics in patients undergoing laparoscopic surgery for benign gynecological tumors. Systems Medicine, 2023, 8(17): 178-181.
Ye HL. Comparison of the effect of dexmedetomidine combined with remifentanil and propofol on hemodynamics in patients undergoing hysteroscopic surgery under anesthesia. Famous Doctor, 2023, 20(2): 168-170. - Ye H, Ouyang J. Effect of dexmedetomidine combined with dezocine anesthesia on sedation, analgesia and hemodynamics in patients undergoing laparoscopic gynecological surgery. Primary Medical Forum, 2023, 27(31): 71-73, 77.
- Chen Q. Effect of dexmedetomidine combined with general anesthesia on hemodynamics and Ramsay sedation score at different time points after anesthesia induction in elderly patients with femoral neck fracture. Sichuan Journal of Physiological Science, 2023, 29(9): 225-227.
- Hu R. Effect of dexmedetomidine hydrochloride and midazolam on hemodynamics and recovery quality in elderly patients undergoing thoracic surgery under general anesthesia. Henan Journal of Surgery, 2023, 29(1): 88-91.
- Lin LF, Rao XC. Effect of low-dose dexmedetomidine on hemodynamics during recovery and extubation period in elderly hypertensive patients undergoing elective general anesthesia. Journal of Chronic Diseases, 2023, 24(11): 1642-1645.
- Li BK, Wang JY, Zhu Y. Effect of low-dose dexmedetomidine combined with propofol on hemodynamics and analgesic effect in elderly patients undergoing laparoscopic cholecystectomy. Geriatrics and Health Care, 2022, 28(4): 146-149.
- Wang X. Effect of dexmedetomidine combined with epidural anesthesia on stress response indicators, respiratory and circulatory indicators, and cognitive function in elderly patients undergoing hernia surgery. Clinical Medical Research and Practice, 2022, 7(9): 101-104.
Share this Articles