Effect of dexmedetomidine on neurological and cognitive functions and inflammatory factor expression in elderly patients undergoing knee arthroplasty
Xiao-ying Xie, MSMS1, Bo Gao, MSMS1, Bing-qiang Zheng, MSMS1, Meng Meng, MSMS1, Qi-wei Zhang, MSMS1*
1 Department of Anesthesiology, Hebei PetroChina Central Hospital, Langfang, China. *Corresponding authors at: Department of Anesthesiology, Hebei PetroChina Central Hospital, Langfang, Hebei 065000, China. E-mail addresses: qiwei@qq.com (Q. Zhang).
Abstract
Background: Total knee arthroplasty (TKA) in elderly patients with osteoarthritis can lead to inflammation and postoperative cognitive dysfunction (POCD). Dexmedetomidine may reduce these adverse effects, but the optimal dosage to minimize postoperative complications is still under investigation.
Objective: This study aims to investigate the effects of dexmedetomidine on neurological function, cognitive function, and inflammatory factor expression in elderly patients undergoing knee arthroplasty.
Methods: A total of 120 elderly patients who underwent unilateral total knee arthroplasty (TKA) from March 2022 to March 2023 were enrolled and divided randomly into four groups (A, B, C, D), each with 30 patients. Group A received combined spinal-epidural anesthesia, while groups B, C, and D received additional dexmedetomidine at a loading dose of 0.5 μg/kg, followed by continuous intravenous infusion at rates of 0.30, 0.50, and 0.80 μg/(kg·h), respectively. Serum levels of inflammatory factors, markers of brain tissue injury, and Montreal Cognitive Assessment Scale (MoCA) scores were compared before and after surgery among the groups. Postoperative cognitive dysfunction (POCD) and adverse events were also recorded.
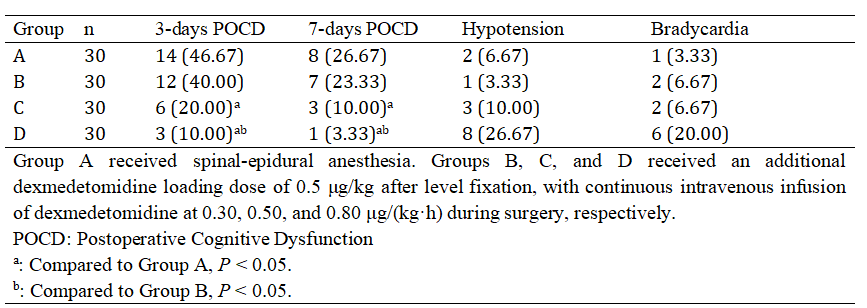
Results: Serum TNF-α, IL-6, and IL-10 levels in all groups were higher at 1 hour, 1 day, and 3 days post-surgery than pre-surgery (P < 0.05). Serum S-100β and ICAM-1 levels increased post-surgery in all groups but were significantly lower in group D than in groups A, B, and C, and lower in group C than in groups A and B (P < 0.05). MoCA scores in groups A and B at 1, 3, and 7 days post-surgery were lower than pre-surgery (P < 0.05). MoCA scores in groups C and D decreased at 1 and 3 days post-surgery but returned to preoperative levels by day 7. MoCA scores in group D were higher than those in groups A, B, and C at 1, 3, and 7 days post-surgery, and higher in group C than in groups A and B (P < 0.05). The incidence of POCD on day 3 post-surgery was lower in group D than in groups A and B and lower in group C than in group A (P < 0.05). There was no significant difference in hypotension or bradycardia among the four groups (P > 0.05).
Conclusions: Continuous intraoperative infusion of dexmedetomidine at a rate of 0.80 μg/(kg·h) significantly reduces postoperative inflammatory, neurological, and cognitive injuries in elderly patients undergoing knee arthroplasty, ensuring anesthesia safety.
Trial registration: Not applicable.
Keywords: Dexmedetomidine; Anesthesia; Knee arthroplasty; Tumor necrosis factor-alpha; Interleukin-6; Cell adhesion molecule-1; Astrocyte-derived protein; Cognitive dysfunction
Introduction
Knee osteoarthritis is a degenerative joint disease primarily affecting the elderly. Total knee arthroplasty (TKA) is often performed to treat severe cases, but this invasive procedure can trigger a significant inflammatory response and stress reaction due to the implantation of prosthetic materials, potentially leading to neuronal damage and postoperative cognitive dysfunction (POCD). Combined spinal-epidural anesthesia is commonly used due to its effective muscle relaxation and rapid onset, yet postoperative stress responses may persist, and it has limited effects on alleviating patient anxiety, increasing the risk of central nervous complications post-surgery.
Dexmedetomidine, known for its protective effects on the cardiovascular system, can mitigate the neurotoxic effects of anesthetics, reduce neuronal apoptosis, and lower the incidence of POCD. However, there is currently no standardized clinical dosage for dexmedetomidine. Research is ongoing to evaluate whether increasing the dexmedetomidine dose can further reduce postoperative inflammatory, neurological, and cognitive injuries.
This study evaluates the effects of different doses of dexmedetomidine on inflammatory response, neuronal injury, and cognitive function in elderly patients undergoing TKA.
Methods
Patient Selection
This prospective study included 120 elderly patients who underwent elective unilateral TKA from March 2022 to March 2023 at Hebei PetroChina Central Hospital. Patients were randomly divided into four groups: A, B, C, and D, each with 30 participants. Gender, age, BMI, disease duration, education level, surgery time, ASA classification, affected side, and intraoperative blood loss were comparable among groups (P > 0.05).
Table 1. Comparison of general information among four groups
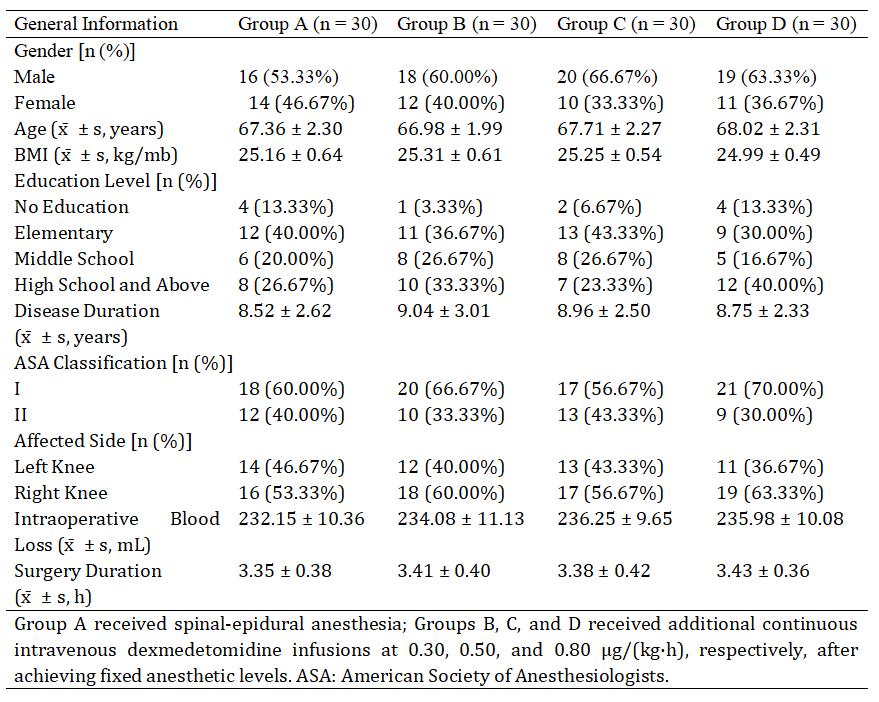
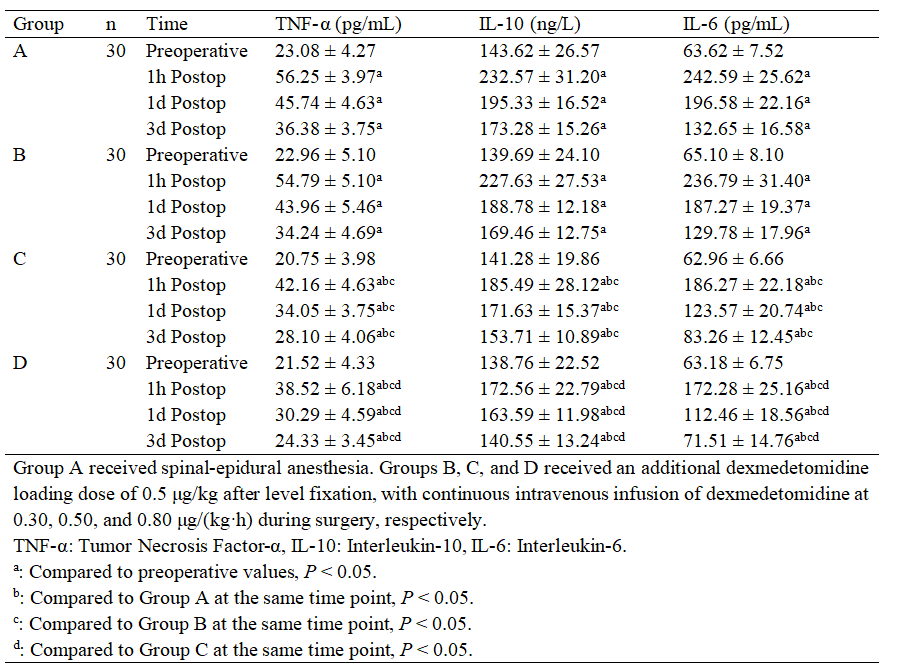
Table 2. Comparison of serum inflammatory factors before and after surgery among four groups
Inclusion criteria included a confirmed diagnosis of knee osteoarthritis, eligibility for elective TKA, age between 60 and 75, acceptance of combined spinal-epidural anesthesia, and an ASA classification of I or II. Patients with severe liver or kidney dysfunction, hematologic or cerebrovascular diseases, psychiatric disorders, or allergies to the study medications were excluded.
Anesthesia Protocol
After IV access was established, patients were given supplemental oxygen and monitored for vital signs. Group A received combined spinal-epidural anesthesia with 0.75% ropivacaine, while groups B, C, and D received additional dexmedetomidine. After a loading dose of 0.5 μg/kg, dexmedetomidine was administered via continuous IV infusion at rates of 0.30, 0.50, and 0.80 μg/(kg·h), respectively, starting after stable fixation of the anesthesia plane.
Postoperative analgesia was provided through IV self-controlled analgesia using a solution of 1% ropivacaine, sufentanil, and tropisetron in saline.
Observational Indicators
Inflammatory factor levels: Serum samples were collected at baseline, 1 hour, 1 day, and 3 days post-surgery to assess levels of TNF-α, IL-6, and IL-10 via ELISA.
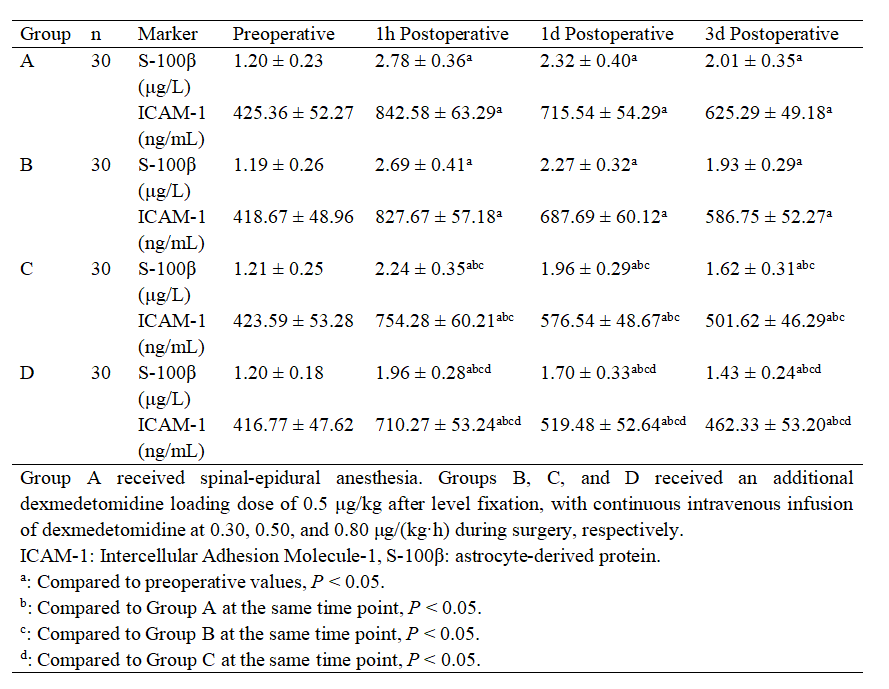
Markers of brain injury: Levels of ICAM-1 and S-100β were measured in serum samples to evaluate brain tissue damage.
Cognitive function: Cognitive status was assessed using the Montreal Cognitive Assessment Scale (MoCA) on days 1, 3, and 7 post-surgery. MoCA evaluates multiple cognitive domains, with scores adjusted for education level.
POCD and adverse events: Incidences of POCD (MoCA <27), hypotension, and bradycardia were recorded for each group on days 3 and 7 post-surgery.
Statistical Analysis
Data were analyzed using SPSS 22.0. Quantitative data were expressed as mean ± standard deviation, with comparisons among groups performed using ANOVA and paired t-tests. Categorical data were expressed as percentages, and chi-square tests were used for comparisons. A significance level of α = 0.05 was applied.
Table 3. Comparison of brain tissue injury markers before and after surgery among four groups
Results
Inflammatory Factors
Preoperative inflammatory factor levels showed no significant differences among groups (P > 0.05). However, TNF-α, IL-6, and IL-10 levels at 1 hour, 1 day, and 3 days post-surgery were significantly lower in group D compared to groups A, B, and C, and lower in group C compared to groups A and B (P < 0.05).
Brain Injury Markers
ICAM-1 and S-100β levels were significantly elevated post-surgery across all groups but were consistently lower in group D than in groups A, B, and C, and lower in group C than in groups A and B (P < 0.05).
Table 4. Comparison of MoCA scores before and after surgery among four groups
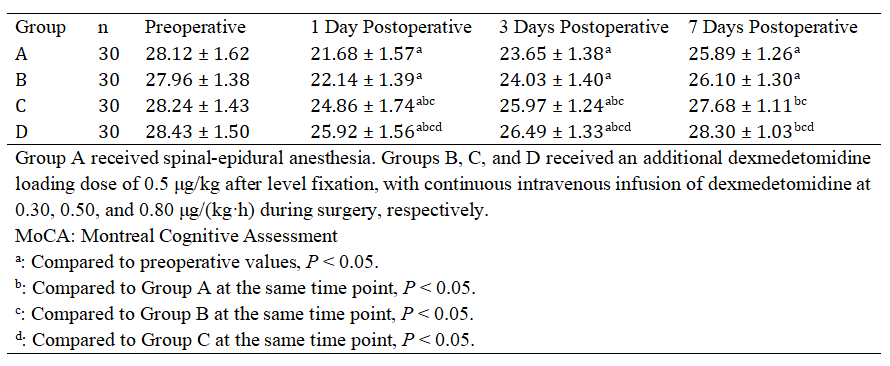
Table 5. Comparison of POCD and incidence of adverse reactions before and after surgery among four groups
Cognitive Function (MoCA Scores)
MoCA scores in groups A and B were significantly lower than preoperative levels at days 1, 3, and 7 post-surgery. Groups C and D showed similar declines at days 1 and 3 but returned to baseline by day 7. MoCA scores were higher in group D than in groups A, B, and C, and higher in group C than in groups A and B at all postoperative time points (P < 0.05).
Cognitive Function (MoCA Scores)
On day 3 post-surgery, POCD incidence was significantly lower in group D compared to groups A and B, and lower in group C than in group A (P < 0.05). There were no significant differences in hypotension or bradycardia incidence among the groups (P > 0.05).
Discussion
Total knee arthroplasty (TKA) is a traumatic surgery for treating degenerative knee disease in the elderly, commonly performed under combined spinal-epidural anesthesia (3). However, surgical trauma, advanced age, and insufficient sedation or analgesia may contribute to postoperative cognitive dysfunction (POCD) (11-12). Reducing POCD incidence post-TKA in elderly patients has become a significant clinical challenge. Studies show that dexmedetomidine provides effective sedation and analgesia, reducing POCD occurrence in elderly patients, though the optimal dose is still under investigation (13-14). Research by Fan Yuhong et al. found that continuous infusion at rates of 0.50 and 0.80 μg/kg per hour mitigated inflammatory responses and lowered POCD rates in elderly patients (11). Similarly, Wang Haili et al. reported that 0.50 μg/kg dexmedetomidine stabilized hemodynamic levels during anesthesia in elderly hip replacement patients, reducing cognitive impairment with reliable safety (12). Peng Bei's study also demonstrated that 0.30 μg/kg continuous infusion reduced POCD rates in elderly hip replacement patients (15). Therefore, this study compares dexmedetomidine continuous infusion doses of 0.30, 0.50, and 0.80 μg/(kg·h) with standard anesthesia (Group A) to assess efficacy.
Our findings indicate that dexmedetomidine effectively reduces postoperative neurological and cognitive injuries in elderly TKA patients, with the 0.80 μg/kg per hour infusion achieving the best results. This may be due to dexmedetomidine’s stimulation of α receptors on arterioles and pial arteries, leading to vascular constriction, reduced local blood flow, and improved cerebral oxygenation. This protective effect on brain tissue may also be linked to its activation of PI3K/Akt and inhibition of the p38/MAPK signaling pathways, as well as increased expression of brain-derived neurotrophic factor (BDNF) through the JAK/STAT pathway, which collectively mitigates cognitive impairment (16-17). Higher doses of dexmedetomidine demonstrate stronger effects and more significant improvements (18-20).
Additionally, dexmedetomidine significantly reduces postoperative inflammatory responses in elderly TKA patients, particularly with the 0.80 μg/(kg·h) infusion, consistent with Fan Yuhong's findings (11). This effect is likely due to dexmedetomidine's inhibition of excessive macrophage activation, reducing inflammatory cytokine release and controlling inflammation-related damage, with evidence suggesting that higher doses correlate with better anti-inflammatory effects (21-22). In our study, both 0.50 and 0.80 μg/(kg·h) infusions lowered POCD rates, with the 0.80 μg/(kg·h) dose proving most effective. Inflammatory cytokines are a known risk factor for POCD, and the superior anti-inflammatory and neuroprotective effects of the 0.80 μg/(kg·h) dose likely contribute to reduced POCD incidence (23-25).
However, the 0.80 μg/(kg·h) dose was associated with an increased incidence of hypotension and bradycardia, possibly due to dexmedetomidine's suppressive effects on sinoatrial and atrioventricular node functions, potentially prolonging recovery time and triggering hypotension and bradycardia (26). These adverse effects primarily occurred during post-surgery tourniquet release and were effectively managed with atropine or ephedrine, with no significant differences between groups, potentially due to the small sample size in this study.
Despite analyzing different dexmedetomidine doses, limitations include a small sample size and exclusion of patients over 75 with comorbidities who rarely undergo surgery, which may affect results. Further studies are needed to determine if the neuroprotective effects of dexmedetomidine in the elderly are age dependent.
In conclusion, continuous intravenous infusion of 0.80 μg/(kg·h) dexmedetomidine effectively reduces inflammatory, neurological, and cognitive injuries and lowers POCD rates in elderly TKA patients, ensuring clinical anesthesia safety.
Conflicts of Interest:
The authors declare that they have no competing interests.
Abbreviations
Akt: protein kinase B
ANOVA: analysis of variance
ASA: American society of anesthesiologists
BDNF: brain-derived neurotrophic factor
BMI: body mass index
ELISA: enzyme-linked immunosorbent assay
ICAM-1: intercellular adhesion molecule-1
IL-6: interleukin-6
IL-10: interleukin-10
IV: intravenous
JAK/STAT: Janus kinase/signal transducer and activator of transcription
MAPK: mitogen-activated protein kinase
MoCA: Montreal cognitive assessment scale
PI3K: phosphoinositide 3-kinase
POCD: postoperative cognitive dysfunction
S-100β: S-100 beta protein
SPSS: statistical package for the social sciences
TKA: total knee arthroplasty
TNF-α: tumor necrosis factor-alpha
References
- Hu KD, Liu K. Effects of glucosamine sulfate combined with meloxicam on serum FGF-2, TGF-β, and IGF-1 levels and knee joint function in patients with knee osteoarthritis. Clin Misdiagnosis Mistherapy. 2024;37(9):66-70.
- Liang ZQ, Meng QC, Li XS, et al. Correlation between serum PDGF, FGF-2 levels, and the severity of knee osteoarthritis. J Difficult Dis. 2023;22(9):972-976.
- Jain K, Puri A, Taneja R, et al. Preprocedural ultrasound as an adjunct to blind conventional technique for epidural neuraxial blockade in hip or knee joint replacement: a randomized controlled trial. Indian J Anaesth. 2019;63(11):924-931.
- Zhang X, Fu Q. Correlation of cerebrospinal fluid amyloid β-protein 42 and neurofilament light protein levels with postoperative neurocognitive dysfunction in elderly patients. J South Med Univ. 2021;41(4):574-578.
- Weng HJ, Wang HG, Xu CJ, et al. Effects of continuous intravenous dexmedetomidine on postoperative delirium in elderly orthopedic surgery patients. Shenzhen J Integr Tradit Chin West Med. 2022;32(18):75-77.
- Fu LF, Wang JP, Zhong CF, et al. Observation of the effects of dexmedetomidine on anesthesia and blood pressure in elderly orthopedic surgery patients with combined spinal-epidural anesthesia. Basic Med Forum. 2021;25(17):2381-2383.
- Kurup MT, Sarkar S, Verma R, et al. Comparative evaluation of intraoperative dexmedetomidine versus lidocaine for reducing postoperative cognitive decline in elderly patients: a prospective randomized controlled trial. Anaesthesiol Intensive Ther. 2023;55(5):349-357.
- Li Z, Yao S, Cheng M, et al. Evaluation of dexmedetomidine on postoperative cognitive dysfunction through Aβ and cytokine analysis. Iran J Pharm Res. 2021;20(2):515-522.
- Chinese Medical Association, Joint Surgery Committee, Chinese Orthopedic Association, National Geriatric Disease Clinical Research Center (Xiangya Hospital). China Osteoarthritis Diagnosis and Treatment Guidelines. [Updated 2021].
- Ye B, Wei D, Pan L. Montreal Cognitive Assessment for cognitive dysfunction post-basal ganglia stroke. Acta Neurol Belg. 2022;122(4):881-884.
- Fan YH, Zhao Q, Yuan B, et al. Effects of different doses of dexmedetomidine on cognitive function in elderly patients with the APOE ε4 allele after total intravenous anesthesia. Chinese Med J. 2021;56(4):454-457.
- Wang HL, Pan H, Yang AL, et al. Effects of different doses of dexmedetomidine on cognitive function in elderly patients undergoing hip arthroplasty. J Clin Psychosomatic Dis. 2022;28(3):29-34,45.
- Zeng K, Long J, Li Y, et al. Preventing postoperative cognitive dysfunction using anesthetic drugs in elderly patients undergoing noncardiac surgery: a systematic review and meta-analysis. Int J Surg. 2023;109(1):21-31.
- Zhang J, Liu G, Zhang F, et al. Analysis of postoperative cognitive dysfunction and influencing factors of dexmedetomidine anesthesia in elderly patients with colorectal cancer. Oncol Lett. 2019;18(3):3058-3064.
- Peng B, Peng ZY, Zheng LM, et al. Effects of different doses of dexmedetomidine combined with sufentanil on postoperative functional recovery and delirium in elderly patients undergoing hip arthroplasty. Practical Pharm Clin. 2019;22(5):485-488.
- Shan YY, Wang H, Liu HT. Protective effects and molecular mechanisms of dexmedetomidine in neural injury. J China Physicians Adv. 2018;41(1):74-77.
- Chen N, Chen X, Xie J, et al. Dexmedetomidine protects aged rats from postoperative cognitive dysfunction by reducing hippocampal inflammation. Mol Med Rep. 2019;20(3):2119-2126.
- Tang YX, Wang YS, Kong GY, et al. Preventive effects of dexmedetomidine on delirium and early postoperative cognitive dysfunction in elderly patients undergoing liver lobe resection. J Cent South Univ Med Sci. 2022;47(2):219-225.
- Gu XH, Yu W, Yu XY, et al. Effects of different doses of dexmedetomidine combined with propofol on inflammation, oxidative stress, and postoperative delirium in esophageal cancer resection patients. Adv Biomed Prog. 2023;23(8):1584-1589.
- Karthik NM, Das SG, Johney J, et al. Comparison of postoperative analgesia with two doses of dexmedetomidine as an adjuvant to ropivacaine in adductor canal block for unilateral total knee replacement: a randomized double-blinded study. J Anaesthesiol Clin Pharmacol. 2022;38(3):428-433.
- Chen S, Wu J, Li A, et al. Effect and mechanisms of dexmedetomidine combined with macrophage migration inhibitory factor inhibition on the expression of inflammatory factors and AMPK in mice. Clin Exp Immunol. 2023;212(1):61-69.
- MENG Q, GUO P, JIANG Z, et al. Dexmedetomidine inhibits LPS-induced proinflammatory responses via suppressing HIF1α-dependent glycolysis in macrophages [J]. Aging (Albany NY), 2020, 12(10): 9534-9548.
- RUMP K, ADAMZIK M. Epigenetic mechanisms of postoperative cognitive impairment induced by anesthesia and neuroinflammation [J]. Cells, 2022, 11(19): 2954.
- PENG W, LU W, JIANG X, et al. Current progress on neuroinflammation-mediated postoperative cognitive dysfunction: an update [J]. Curr Mol Med, 2023, 23(10): 1077-1086.
- LUO A, YAN J, TANG X, et al. Postoperative cognitive dysfunction in the aged: the collision of neuroinflammation with perioperative neuroinflammation [J]. Inflammopharmacology, 2019, 27(1): 27-37.
- ACHARYA R, SRIRAMKA B, KOUSHIK P. Comparison of dexmedetomidine alone with dexmedetomidine and fentanyl during awake fiberoptic intubation in patients with difficult airway: a randomized clinical trial [J]. J Dent Anesth Pain Med, 2022, 22(5): 349-356.
Share this Articles